Year 3 - Patient-Centered Clinical Experiences Phase
At the start of third year, all students participate in the two-week Transition to Clerkships Course (T2C2) course that provides support and skills in moving toward a clinical workplace teaching environment (e.g., clinics, hospitals, operating rooms, emergency departments, labor and delivery, etc.)
Third-year students then have excellent educational experiences as clerkships in the core areas of medicine, surgery, family medicine, pediatrics, obstetrics-gynecology, psychiatry, neurology, and emergency medicine with our clinical affiliates in Inland Southern California. Several curricular threads may continue into year 3 and 4.
They also have the opportunity to take three 2-week electives and also complete a new 2-week Community Advocacy Course. Intersessions will strengthen clinical reasoning, integrate scientific knowledge, topics spanning multiple clerkships, and facilitate reflection on their clinical experiences and personal growth.
At the end of year 3, students present a capstone LACE health systems science project and have their clinical skills assessed as part of the California Clinical Performance Examination (CPX). Students take USMLE Step 2CK at the end of third year or beginning of fourth year.
Other enhancements include:
- New formative and summative observed structured clinical encounters and simulation within clerkships.
- Graduation-requirement assessments tied to mission-aligned competencies (e.g., advocacy skills, value-based care skills, culturally responsive care, etc.).
- Enhanced instruction in high-impact Step 2 CK areas.
- Maintaining wellness days.
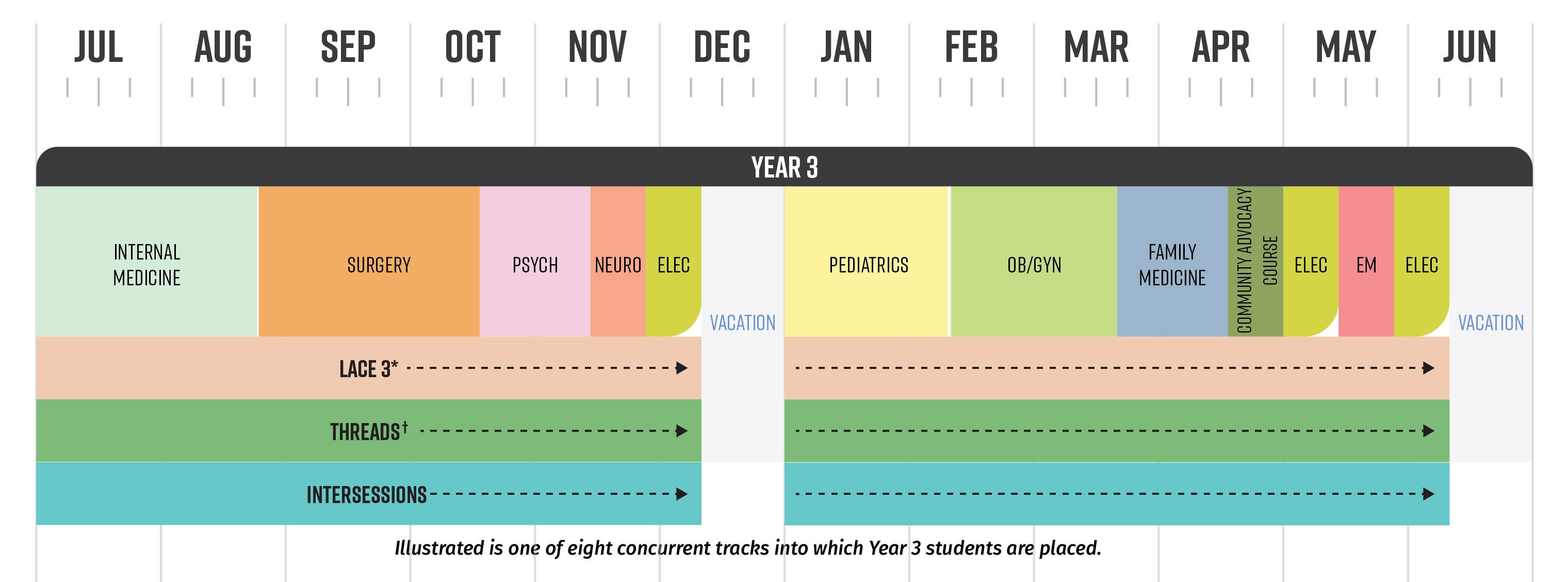
Year 3 Schedule
- Transition to Clerkships course (2 weeks)
- Community Advocacy course (2 weeks)
- Clerkship blocks
- Internal Medicine (8 weeks)
- Surgery (8 weeks)
- Pediatrics (6 weeks)
- Obstetrics and Gynecology (6 weeks)
- Family Medicine (4 weeks)
- Emergency Medicine (2 weeks)
- Psychiatry (4 weeks)
- Neurology (2 weeks)
- Longitudinal Experiences
- LACE 3
- Intersessions
- Curricular threads
- Educational Enhancement Experiences
- 3 electives (2 weeks each)
Community Advocacy Course
The Community Advocacy Course teaches the skills to best support health equity for individual patients, families, communities, the region, state and the nation.
This integrated mission-based course will feature health-systems science content (e.g., quality and safety, medical economics and stewardship), HESJAR approaches in clinical care, social medicine and social justice efforts by physicians in community and public health arenas especially vulnerable populations.
There will be opportunities for interprofessional collaboration between MD and MPH students.
Intersessions
The third year of medical school is a period of great professional and personal growth, but is also a huge time commitment that can be socially isolating and make it difficult to find time for introspection. Intersessions will help address this.
Students explore:
- Integration of four science pillars.
- Clinical sciences
- Basic sciences
- Health systems sciences
- Behavioral sciences
- Application of evidence-based medicine skills.
- Clinical context for basic science concepts.
- How basic science concepts to help inform more effective clinical decision.
- Integration of topics between clerkship specialties. Examples include:
- Diagnosis and management of depression in primary care, emergency care and mental health care settings.
- Optimizing maternal fetal health outcomes.
- Medical clearance of a pre-surgical patient.
- Interprofessional team care.
- Via Balint groups, students will meet with trained facilitators to discuss challenging or emotionally-charged cases that feel unresolved, confusing, or frustrating. Sessions focus on the emotional aspect of the doctor patient relations. Through private group discussions, new insights and perspectives emerge, enhancing self-awareness and effectiveness in clinical practice. This will enhance student resilience.